“What brings you in today?”
The pause before answering that question is not uncommon, and it’s rarely easy to answer.
How do we talk when we talk about pain? And how do we talk to others about our pain? More so—how do we talk to our doctors about pain? Making sure that our doctors take our pain seriously is critical as we look to them for guidance on how to improve our pain or eliminate its source.
Is there specific pain terminology we should be using? A secret language about pain that makes it easier to relate? Or are our senses and memories easier to reference when trying to convey the distinct and direct pangs experienced during bouts of chronic pain?
These are the questions that keep us up at night.
Thankfully, there are many pain assessment tools that exist to help patients and doctors talk about experiencing and managing pain. Understanding the common phrases and practices used to quantify and qualify pain will make sure you’re prepared to talk about it when appointment time comes.
the pain scale
Pain is inherently subjective, so finding a common ground for discussing its impact is crucial. There are several different pain scales that your doctor may use. The Numeric Rating Scale (NRS-11) was invented by Dr. Ronald Melzack and Dr. Warren Torgerson of McGill University. Derived from the McGill Pain Questionnaire, the NRS-11 is an 11-point scale for patient self-reporting of pain. These 11 points on a spectrum range from zero to 10, with zero denoting no pain and 10 denoting the worst pain imaginable. All points are based on the ability for persons 10 years or older to perform daily activities.
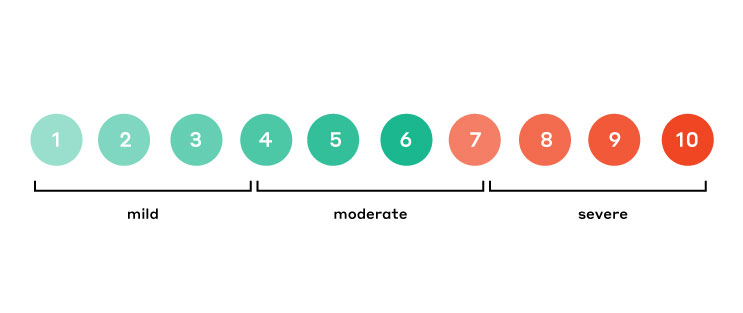
This scale lets doctors and patients speak about pain in a common, simplified language. “On a scale of one to 10, how much does it hurt?” This question becomes much easier to answer and creates a solid starting point for continued conversation about managing and alleviating pain.

For children, there’s the addition of the Wong-Baker FACES® Pain Rating Scale, which adds a visual element to the pain scale and allows children to align their feelings to an expressive face.
Of course, qualifying that pain becomes even more important once you’ve established its quantitative level.
common pain terminology
Is it a sharp pain or a dull pain? Is it burning or tingling? After establishing the level of pain, being able to articulate the kind of pain may help narrow down treatment options or solutions.
Here’s a list of common terms used when talking about pain:
|
|
With the above words as tools you can more easily describe your situation. For example, “It feels sharp and stabbing. It’s like a lightning bolt that pierces quickly without warning.” Or even, “My arm is constantly aching and tender to the touch. It feels like pins and needles that don’t quit.”
Sentences like these provide more context as to the duration of the pain, the sensation and the degree to which the feeling persists. When describing how you feel, make sure you’re also able to communicate:
- How long you’ve had the pain
- Where the pain is located
- When the pain is present—is it constant, or does it come and go?
- What activities aggravate the pain, trigger the pain, or soothe the pain
medical pain terminology
To get even more detailed, you can move beyond the common terms and use more clinical pain terms. Combining a common language of pain with medical terminology will set you up for a successful conversation during appointments. For example, there is more than one type of pain, medically speaking:
- Acute: a sudden onset of pain that usually lasts for a short period of time
- Chronic: a condition that lasts for a long time, it can be constant or intermittent
- Visceral: pain related to the internal organs in the midline of the body
- Somatic: pain that occurs in tissues such as the muscles, skin or joints
- Myofascial: pain and soreness in the muscles
- Breakthrough: pain that occurs suddenly or as a result of a specific activity
- Inflammation: a reaction of tissues to injury or disease; commonly manifests as swelling, redness, heat and pain
There are plenty of other terms used in the universe of pain management. Many are documented in pain management glossaries and online reference materials.
advocating for yourself
Armed with the right tools to talk about pain, you’ll be better equipped to communicate what you are feeling and how it impacts your day-to-day life. Bring in notes and write out any questions you may have ahead of time so you’re ready to ask, listen, and make a plan to move forward toward a pain-free solution.
navigating nerve pain
When you’re ready to talk to a doctor about pain, we may be able to help. If your chronic pain started after a traumatic injury, surgery, or amputation, it could be the result of nerve damage. Take the quiz to see if you’re a potential candidate for surgical nerve repair.