 Shirley was born just before the polio vaccine was widely available and contracted the disease when she was about 3 years old. This set the wheels in motion for a lifetime of surgeries, doctor appointments and eventual chronic pain.
Shirley was born just before the polio vaccine was widely available and contracted the disease when she was about 3 years old. This set the wheels in motion for a lifetime of surgeries, doctor appointments and eventual chronic pain.
As a child, she underwent multiple surgeries to correct deformities in her lower leg and foot. Unknowingly, these surgeries caused trauma and injury to the nerves in her leg.
But polio didn’t break her spirit. Shirley was determined, or “stubborn” as she would say, to live a life just like all others around her—full and happy and active. Her irritation at not being invited to play in sports developed into a drive to show the world that she was capable.
And she did just that. Shirley grew up, fell in love, started a successful career, and flourished in spite of her childhood illness.
But one day, things changed.
a new kind of pain
 “One day, in 2007, I was just sitting in my office and I had [this pain occur]. Since I was a child, I’ve experienced a lot of pain [due to polio], but nothing like this. So, I thought, ‘Well, OK, it will just go away.’”
“One day, in 2007, I was just sitting in my office and I had [this pain occur]. Since I was a child, I’ve experienced a lot of pain [due to polio], but nothing like this. So, I thought, ‘Well, OK, it will just go away.’”
“I’ve had pain before, but I’ve not had pain like this.”
But it didn’t. The pain stayed, and the pain progressed. And for six years, Shirley didn’t have an answer as to why it was there.
“At first, I [hoped] it would go away, because I really didn’t want to go in for another surgery on my leg,” Shirley said. “So, I would come home from work really late, and Danny, my husband, would be there with my dinner and the pain pills. And then I would just get in bed and the pain pill would take effect, and then I would have some relief for a while.”
Due to her pain, Shirley retreated from friends, family and her social life. The pain made it hard to enjoy things that she once did.
“I’m a very social person and I like to be around people and do things with friends and family. But I retreated because the pain was so bad. The pain didn’t take a weekend off. So, I just kind of became a hermit and family would say, ‘Well, why don’t you come and visit?’ And I wanted to say, ‘Do you know how much work it is to get myself out of bed, and go travel to a family member’s house, or a friend’s house, and not sit there and writhe in pain?’ It just wasn’t worth it to me.”
“I felt that I had really lost one of the most important aspects of my life that I loved. I was really, really angry at this pain for a long time.”
But Shirley’s stubbornness wouldn’t let her give up. “I thought, ‘Well, this is ridiculous. I’m not going to live the rest of my life like this. It’s gone on too long.’ So I contacted my podiatrist at the time and told them what was happening.” Her podiatrist had performed several previous surgeries for Shirley over the past decade or more.
exploring all options
Her podiatrist suggested that it was probably time for another reconstructive surgery, and that’s what was causing the pain. “I didn’t know any better. So, I went through the surgery, and it was good to have it for some reconstructive reasons, but it didn’t cure the pain,” Shirley said.
“I can’t live like this, I won’t live like this, so we need to figure out something that will work.”
So, she continued to take the pain medication and tried to go about her life—but she was in chronic pain. So, she contacted her doctor again about a year later.
“I told him ‘I can’t live like this, I won’t live like this, so we need to figure out something that will work.’ And he examined me again and he said, ‘OK, I’m going to send you for an epidural in your back and that’ll shoot pain medication down to your foot.’”
Shirley was referred to a pain management doctor, and she had the epidural.
“I was told that the epidural would give me pain relief from anywhere from six months to a year or longer, because that’s typical for most patients who were experiencing pain. Well, this particular epidural lasted maybe three weeks. So, I contacted my podiatrist again and said ‘That didn’t work, and I’m out of answers. Help me figure this out.’”
And that’s when her doctor of 10 or 15 years suggested amputating her toes. When Shirley didn’t agree right away, her doctor stood up, took her by the elbow and said, “I’m sorry. Shirley, there’s nothing else I can do for you. I wish you a happy, pain-free life.”
an amputation
 “I was pretty much dismissed, and that made me angry because it’s like, it’s your job to help me figure it out. So, I thought, ‘That’s OK, I’ll find somebody else.’”
“I was pretty much dismissed, and that made me angry because it’s like, it’s your job to help me figure it out. So, I thought, ‘That’s OK, I’ll find somebody else.’”
Shirley visited other podiatrists to get a second opinion. One suggested putting pins in her toes and said they didn’t need to be amputated. Another agreed with Shirley’s first podiatrist, that the amputation of the two toes would be the best. And he also agreed that was the source of her pain.
Shirley went through with the surgery and the amputation took the tips of two toes. And the doctor said the pain should be gone within a few weeks. After her surgical pain subsided, the chronic pain shouldn’t return.
“I’m sorry. I don’t know what else I can do for you.”
“Well, the chronic pain returned as soon as the anesthesia had worn off, which was the next day. And on top of that, I had surgical pain because it’s kind of a big deal to have some body parts removed. And so, I called the doctor and I said it didn’t take care of the pain,” explains Shirley. “And he said, ‘Well, I’m sorry. I don’t know what else I can do for you.’”
It was at this point that Shirley thought, “If they can amputate toes, they can amputate a foot.”
a resignation
With her fate somewhat sealed, and the pain staying put, Shirley decided to retire early.
“I retired because I couldn’t stand the pain anymore.
“And I was at my job for 20 years as an executive managing the human resources function of the company. And it was a very demanding job. But [after the pain started] my life, just kind of went on hold. And so I decided one day, ‘I can’t stand this, I’m just going to retire,’ and I gave them my resignation.”
Shirley also resigned herself to life without a foot. Though she hadn’t shared this decision with her husband, she started Googling to find the right doctor for her needs.
“I didn’t tell anybody. I didn’t tell my husband. I didn’t tell my family members or friends because I didn’t want anybody to talk me out of it.”
“The first hit that I got was a team of doctors, one who was a podiatrist in Chicago and the other one who was a neurologist, and they worked in tandem. And I saw that they did all of these very complicated procedures, so I thought, ‘Well, if they know how to do all these things, certainly they know how to take off my foot.’ So, I made an appointment with them.”
At the appointment, Shirley and her husband sat in the office and the doctor asked her, “What is your pain level on a scale of one to 10 right now?”
“And I didn’t even answer that. I said, ‘I’m here because I want you to amputate my foot. It’s just, I can’t live with this anymore.’ Well, my husband was shocked. The doctor laughed and said, I’m not going to do that, but I have a feeling I know what’s wrong with your foot.”
a different diagnosis
From the start, this doctor was different. Working with a neurologist as his partner, they ran tests and talked to Shirley and really got to know and understand her situation. After a couple of visits, she went back to him and he said, “I’ve got the answer.”
The source of Shirley’s pain was three neuromas (tangled masses of scar tissue) in the nerves of her lower legs likely caused by her previous surgeries from years ago. Nothing that she had tried before would have made a difference, because it wasn’t removing and repairing the source of the pain. Her doctor let Shirley know that this time, she could be helped. Through surgical nerve repair, he could identify and remove the neuromas sending pain signals to the brain. From there, he could repair the resulting nerve gaps using nerve grafts from donor tissue as a bridge to allow the nerves to heal and restore more normal signals. “I’m reasonably certain removing the neuromas and then repairing the nerve will be a solution for you,” he said.
“I had so many conflicting emotions because it’s like, ‘Are you kidding, me?’ Because I had to tell him, you know, I’ve heard it all before, ‘If I do this procedure, I can fix your pain,’ and that’s not necessarily true in my experience. I was skeptical and I was a little bit angry, but I was also very, very, very curious.”
“Transplanting human donor nerve tissue was something I had never heard about before.”
Shirley looked into the procedure and learned more about what it meant to be trained in surgical nerve repair. She learned about the process involved, and how human donors make it all possible. It was new, but it was promising.
With nothing else to lose, Shirley had the surgery on Friday, Dec. 13, of 2013. It was a seven-and-a-half-hour procedure, and Shirley woke up the next day thinking the pain would return along with the surgical pain. But she says, “I haven’t had it since.”
pain free after all this time
 “I fully expected the pain to return because I was still skeptical.”
“I fully expected the pain to return because I was still skeptical.”
“Every day I kept waiting for the pain to return, and every day my husband would ask ‘Any pain?’ And I would say ‘No, I don’t get it,’” said Shirley. “This hadn’t happened before, and it took me a little bit of time, but it finally hit me that it was not coming back … I was over the moon.”
“My husband is my biggest cheerleader and my biggest supporter. He is. He’s been an incredible support person for me through this entire journey. And so have our families and my two best friends.”
And now? Shirley says, “Now I can do everything that I used to do before. I can do all the fun stuff and all the necessary stuff.”
becoming an advocate
Shirley knows that it is not without help that she got where she is. “I thank my donor and my donor’s family every single day for the gift that they gave me, because without them, I don’t know where I would be. There was a couple of thoughts of suicide in there, too, which I never told my husband at the time. So, I’m just incredibly grateful for that donor and their family.”
Since her recovery, Shirley has become an incredible advocate for organ and tissue donation because of the impact that donated nerve tissue had on her life. She’s a volunteer and educates others on the importance of organ and tissue donation.
Becoming an advocate for others seemed like a natural progression after learning to advocate for herself. Shirley says, “Become your own advocate. If you’re not seeing the relief that you’re looking for, don’t necessarily say ‘yes’ to all these different surgeries. Instead, do some of your own research … It’s quite important that you become your own advocate and you find your solution.”
Each patient outcome is dependent upon the nature and extent of nerve loss or damage, the timing between nerve loss and repair, and the natural course of the patient’s recovery. These testimonials reflect the experience of the particular individual and may not represent typical results.
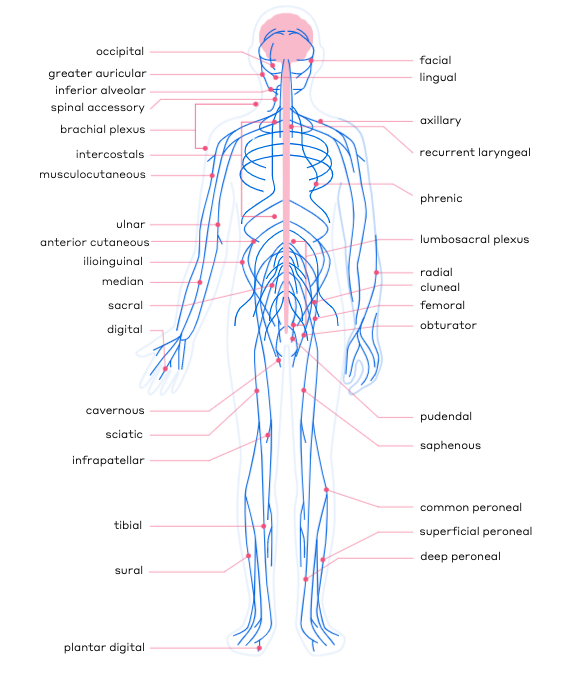 Simply put, nerve surgeons specialize in the surgical repair of peripheral nerves, but since nerves run throughout every inch of our bodies, there is not one specific type of surgeon or title that aligns precisely with the specialty of nerve surgery. Instead, there are several types of doctors who specialize in nerve repair. These doctors undergo extensive microsurgical training to become experts in their field.
Simply put, nerve surgeons specialize in the surgical repair of peripheral nerves, but since nerves run throughout every inch of our bodies, there is not one specific type of surgeon or title that aligns precisely with the specialty of nerve surgery. Instead, there are several types of doctors who specialize in nerve repair. These doctors undergo extensive microsurgical training to become experts in their field.











 Shirley was born just before the polio vaccine was widely available and contracted the disease when she was about 3 years old. This set the wheels in motion for a lifetime of surgeries, doctor appointments and eventual chronic pain.
Shirley was born just before the polio vaccine was widely available and contracted the disease when she was about 3 years old. This set the wheels in motion for a lifetime of surgeries, doctor appointments and eventual chronic pain. “One day, in 2007, I was just sitting in my office and I had [this pain occur]. Since I was a child, I’ve experienced a lot of pain [due to polio], but nothing like this. So, I thought, ‘Well, OK, it will just go away.’”
“One day, in 2007, I was just sitting in my office and I had [this pain occur]. Since I was a child, I’ve experienced a lot of pain [due to polio], but nothing like this. So, I thought, ‘Well, OK, it will just go away.’” “I was pretty much dismissed, and that made me angry because it’s like, it’s your job to help me figure it out. So, I thought, ‘That’s OK, I’ll find somebody else.’”
“I was pretty much dismissed, and that made me angry because it’s like, it’s your job to help me figure it out. So, I thought, ‘That’s OK, I’ll find somebody else.’” “I fully expected the pain to return because I was still skeptical.”
“I fully expected the pain to return because I was still skeptical.”